Back Pain Treatments in Beverly Hills
Lumbar Radiculopathy
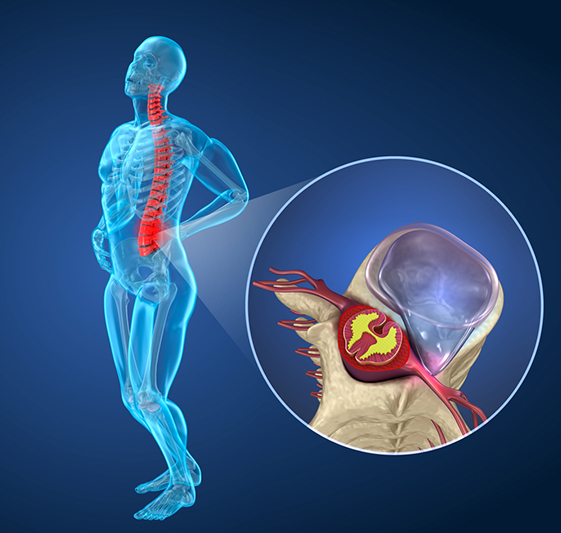
What is Lumbar Radiculopathy?
Radiculopathy is commonly referred to as a “pinched nerve” in the spine. When a nerve in the lumbar or sacral spine (low back) is compressed, it can result in a range of uncomfortable symptoms (neuropathy) in the lower back or legs that may include numbness, pain, tingling, and weakness.
Causes of Lumbar Radiculopathy
The human spine is typically made up of 33 vertebrae (specialized bones) that protect the spinal cord from trauma or injury. The specific design of these bones allows for the different movements in each part of the spine. The spine is S-shaped to facilitate balance, shock absorption, and flexibility. Moreover, each vertebra is connected to the adjacent one by an intervertebral disc that acts like a joint so that the spine can bend and twist. This intervertebral disc also acts as a shock absorber.
Damage or injury to the intervertebral discs may cause irritation or compression of the nearby nerve roots. Depending on the nerve that is affected, one may experience symptoms in different areas of the legs.
Some of the conditions that may cause radiculopathy include:
- Disc herniations
- Osteophytes (bone spurs)
- Degenerative disc disease
- Lumbar facet arthropathy / spondylosis (spinal arthritis)
- Spinal tumors
- Compression fractures
- Scoliosis or other bone deformities.
Learn more about Lumbar Radiculopathy
Sciatica and Piriformis Syndrome
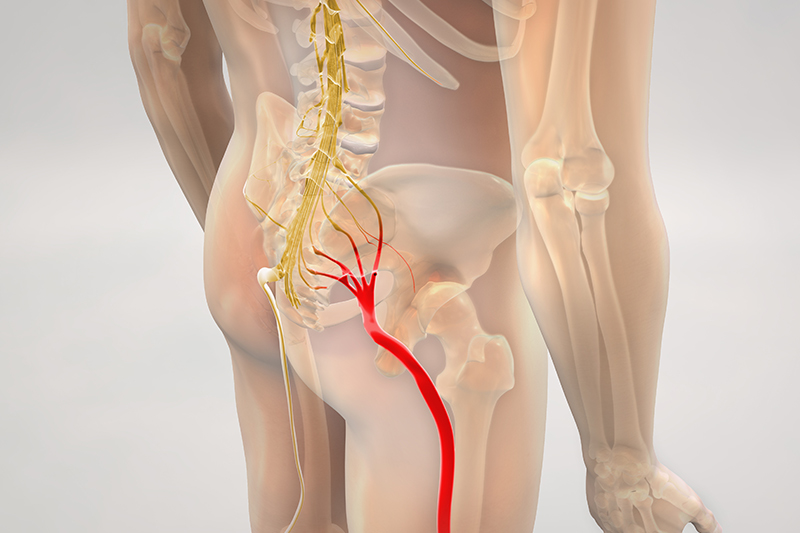
Sciatica refers to pain in the distribution of the sciatic nerve, which starts in the buttocks and travels down both legs. Sciatic pain often gets worse with sitting, especially on hard or uneven surfaces, or with certain activities. Sciatica can be caused by nerve irritation anywhere along the course of the nerve, but is often due to a herniated disc, bone spurs, or soft tissue irritation of the nerve.
Piriformis syndrome is a condition characterized by pain in the buttocks and/or lower back that often radiates to the leg. The condition involves the piriformis muscle in the buttock region. The large sciatic nerve often runs directly next to or through the piriformis muscle, which can cause irritation and compression of the sciatic nerve.
Causes of Piriformis syndrome
This condition is often caused by swelling or spasm of the piriformis muscle which can lead to compression and irritation of the sciatic nerve. Certain structural variations in the anatomy of the sciatic nerve and piriformis muscle can predispose a person to this condition. Often this condition is caused by trauma or sports injuries that involve:
- Trauma to the buttocks
- Strain or sprain
- Overuse injuries
- Hematoma
- Scar formation
Learn more about Sciatica and Piriformis Syndrome
Lumbar Facet Syndrome (Spondylosis, Facet Arthropathy/Arthritis, Spondylitis, Facet Sprain)
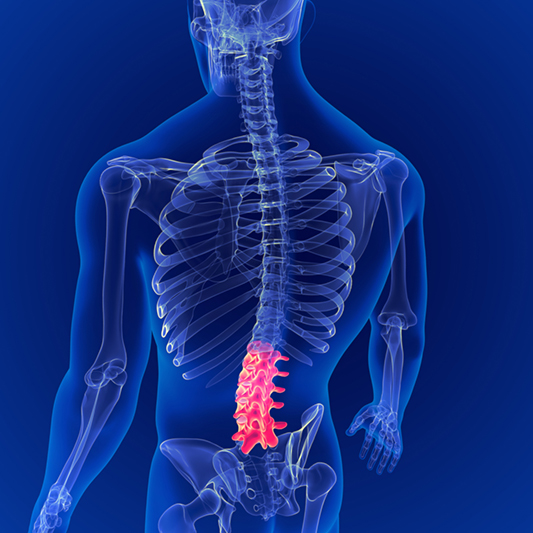
The human spine is made up of vertebrae (bones) that are stacked on top of each other. Each segment is connected in the front by an intervertebral disc and in the back by small facet joints. Damage, irritation, or degeneration of these small facet joints can lead to significant impairments. The painful conditions caused by abnormal function of the facet joints are referred to as facet syndrome.
Causes of Lumbar Facet Syndrome
As people age, the facet joints and discs wear out and degenerate, causing changes that interfere with the normal structure and function of the spine. Spine degeneration is a common aging process, and spinal arthritis may not cause major problems. That being said, some people experience severe low back pain from arthritic facet joints. This painful degenerative spinal condition is referred to as spondylosis, facet disease or facet pain.
Facet syndrome can affect the cervical spine (neck), thoracic spine (upper and middle back), or lumbar spine (lower back). As the discs separating vertebrae shrink (with age or trauma), it places greater forces on the facet joints in the back of the spine causing the bones to rub against each other during spinal movement. This contributes to the changes in the structure and function of the joints.
The facet joints can also cause significant pain without any evidence of degeneration. Often times this is due to inflammation of the facet joint (spondylitis) or a facet joint sprain caused by trauma to joint due to rapid movements of the spine that can occur in accidents or sports injuries.
In cases of trauma, the sudden movement from, for example, a car accident or football tackle can cause the joints to smash against one another. These injuries lead to damage and swelling of the facet joints that is often not detected even on advanced imaging.
Symptoms of Lumbar Facet Syndrome
- Low back pain
- Stiffness in the lower back
- Pain with leaning back/twisting motions
- Pain with standing for long periods
- Pain that radiates to the back of the thighs or buttocks
- Pain with getting up from a seated position
Learn more about Lumbar Facet Syndrome
Discogenic Low Back Pain / Degenerative Disc Disease
The human spine is made up of vertebrae (bones) that are stacked on top of each other. Each segment is connected in the front by an intervertebral disc and in the back by small facet joints. The discs act like shock absorbers in the spine and allow the vertebrae to bend and twist relative to one another. Damage to one or more of these discs can lead to a painful condition referred to as discogenic pain.
Causes of Discogenic Low Back Pain and Degenerative Disc Disease
There are various causes of discogenic low back pain, but most commonly it is caused by trauma or degeneration (wear and tear).
In cases of trauma, such as in a car accident or sports injury, there can be damage or inflammation to the outer layers of the disc leading to disc herniations, bulges, extrusion, prolapse etc. This damage and deformation can cause swelling and pain in the back itself, or cause irritation or compression of a nerve which may result in Lumbar radiculopathy or Lumbar Spinal Stenosis.
Often times discogenic pain may be a result of wear and tear, drying out, and shrinking of the disc over time. In that case it is referred to as degenerative disc disease.
As the process is a slow and gradual decline of the integrity of the disc, degenerative disc disease is often not painful in and of itself, but rather can cause other painful conditions due to the change in the structure and function of the spine. The disc can be gradually pushed into the spinal canal causing Lumbar Radiculopathy or Lumbar Spinal Stenosis. As the discs between the vertebrae shrink, it places greater forces on the facet joints in the back of the spine, causing the bones to rub against each other during spinal movement. This can lead to conditions like Lumbar Facet Syndrome and Lumbar Spondylosis.
Symptoms of Discogenic Low Back Pain
- Back pain with lifting, bending, twisting, or sitting.
- Relief from pain with certain activities or changing positions
- Pain in the low back, buttocks, or thighs
- Intermittent numbness or tingling in the legs
Learn more about Discogenic Low Back Pain
Lumbar Spinal Stenosis

Spinal stenosis is a disorder involving the narrowing of the spinal canal. The spinal canal houses the spinal cord and nerve roots, and narrowing of this passage can cause compression and irritation of these structures.
Causes of Lumbar Spinal Stenosis
Any condition or disease process that takes up space or causes narrowing of the spinal canal can cause spinal stenosis. Some conditions are present at birth or due to developmental abnormalities and may present earlier in life.
Other causes of spinal stenosis are acquired and are either due to trauma, degeneration (wear and tear), disease, or a combination of these. Some of the contributing conditions may include:
- Compression fractures
- Lumbar disc herniation (see Lumbar Discogenic Pain or Lumbar Radiculopathy)
- Lumbar spondylosis with hypertrophy (see Lumbar Facet Syndrome)
- Spondylolisthesis (slippage of a vertebrae)
- Ligamentum flavum hypertrophy (thickening of a ligament in the spine)
- Tumor or neoplasm
Learn more about Lumbar Spinal Stenosis
Thoracic Pain

Thoracic pain refers to discomfort in the upper and middle part of the back or chest. It can involve the thoracic spine, ribs, or the associated muscles and nerves. However, thoracic pain may also be a sign of a problem with an organ such as the heart or lungs, which would require proper evaluation.
Symptoms of thoracic pain may include:
- Upper/mid back pain
- Chest pain
- Feelings of restriction when taking a deep breath
- Pain/Stiffness when twisting the upper trunk
- Pain or pressure on or around the ribs
Learn more about Thoracic Pain
Sacroiliac (SI) Joint Pain
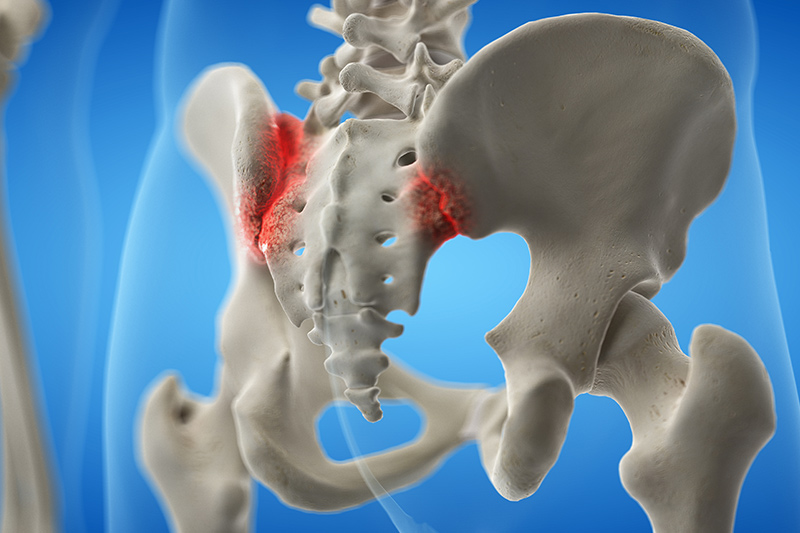
Sacroiliac (SI) joint pain and dysfunction is primarily caused by trauma or degeneration. Like other joints in the body, the SI joint can suffer wear and tear or get injured when there is trauma to the joint or the ligament that supports it. This may cause pain in the lower spine or back, buttocks, pelvis, and legs.
The sacroiliac joint is the part of the low back just below the waist and the top region of the buttocks. It is where the sacrum (bottom of the spine) connects to the iliac bones (pelvic bones). The left and right SI joints have a few degrees of movement when walking and bending. Some common triggers of SI joint pain are accidents or falls. People that suffer from SI joint pain often report that their pain is worse when sitting for prolonged periods of time.
Symptoms of SI Joint Dysfunction
- Pain in the sacroiliac area of the lower back
- Pain after prolonged sitting
- Difficulty bending or twisting the lower back
- Stiffness in the lower back, hip, or leg
- Feeling of being “out of alignment” in the lower back or buttocks
Learn more about SI Joint Pain
Coccydynia/Coccygeal Pain

Coccydynia, which may also be referred to as Coccygeal pain or Tailbone pain, describes a pattern of symptoms that cause persistent or intermittent pain in and around the coccyx (tailbone) area. Coccydynia affects women more often than men as some of the causes are unique to women. The pain may be activity-related or aggravated by sitting especially on hard surfaces. The pain can vary from a sharp pain to mild discomfort in the area.
Symptoms of Coccydynia
The pain may improve with conservative care over the course of a few weeks, but it can turn into a chronic painful condition and can make it difficult to carry out daily activities or sleep. This can result in significant distress, functional limitations and decreased quality of life. This pain may be described as:
- Worse with standing for extended periods, sitting down, sexual activity, or defecating
- Dull with occasional sharp pains
- Worse when sitting on hard surfaces


